Admissions Open: DNB Cardiology Super Speciality Training at TRUST Hospitals, Kakinada

DNB (Super Specialty) – Cardiology
Admissions Open | June 2025 Session
Trust Multispeciality Hospitals, Kakinada – NABH Accredited
Step into a high-volume, high-learning cardiac centre and shape your future as a DNB Cardiology trainee.
⸻
Department Overview
Our dynamic Cardiology programme is supported by a vibrant team consisting of:
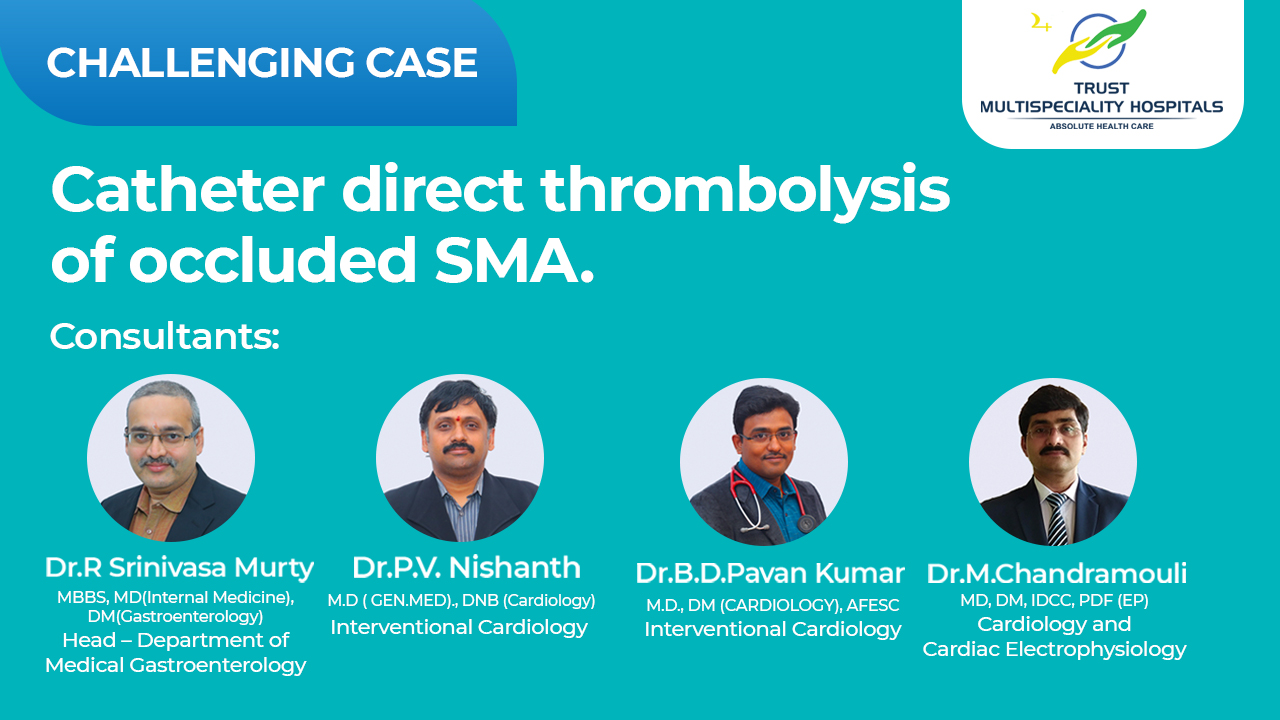
* Two experienced Interventional Cardiologists
* Electrophysiology services
* Paediatric Cardiology services
* Full-fledged CTVS team (Heart-team approach)
We provide comprehensive cardiac care including emergency cardiology, advanced interventional procedures, and non-invasive cardiology under one roof.
⸻
Academic & Clinical Excellence
Train in a modern cardiac unit equipped with:
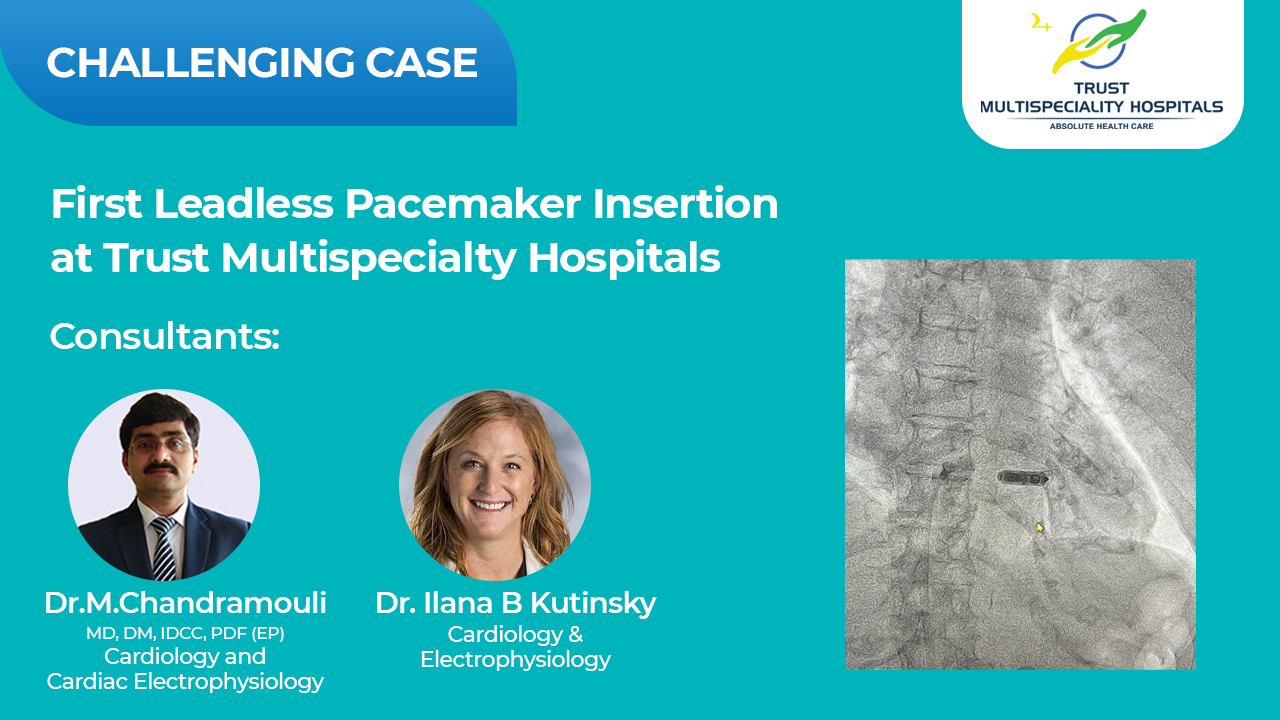
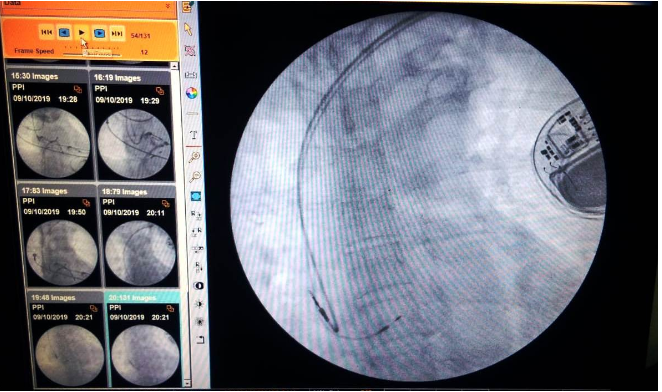
✔️ State-of-the-art Cath Lab
✔️ TTE/TEE for comprehensive cardiac imaging
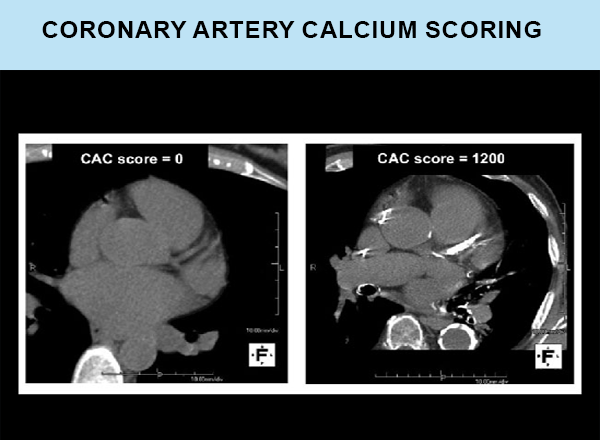
✔️ IVUS & FFR for advanced coronary assessment
✔️ Strong ICU backup for critically ill interventions
✔️ Broad case-mix including structural heart and EP procedures
The program ensures:
* Hands-on procedural exposure from Day 1
* Regular academics – journal clubs, case discussions, cath meets
* Extensive opportunities for assisting & independently performing procedures
* Collaboration with CTVS & ICU for multidisciplinary learning
Ideal for motivated postgraduates aiming to build strong clinical skills and interventional confidence.
⸻
Core Faculty – Cardiology
Dr. P. V. Nishanth
MD (Gen. Med), DNB (Cardiology) – NIMS
Consultant Interventional Cardiologist
+91 98491 35721
Dr. B. D. Pavan Kumar
MD, DM (Cardiology)
Consultant Interventional Cardiologist
+91 93999 92787
Best-in-city cardiology care with dedicated paediatric and EP cardiology services, rapid door-to-needle (20–30 min) and door-to-balloon times (<90 min) in acute MI.
⸻
Key Procedures
* Coronary Angiography
* Coronary Artery Stenting
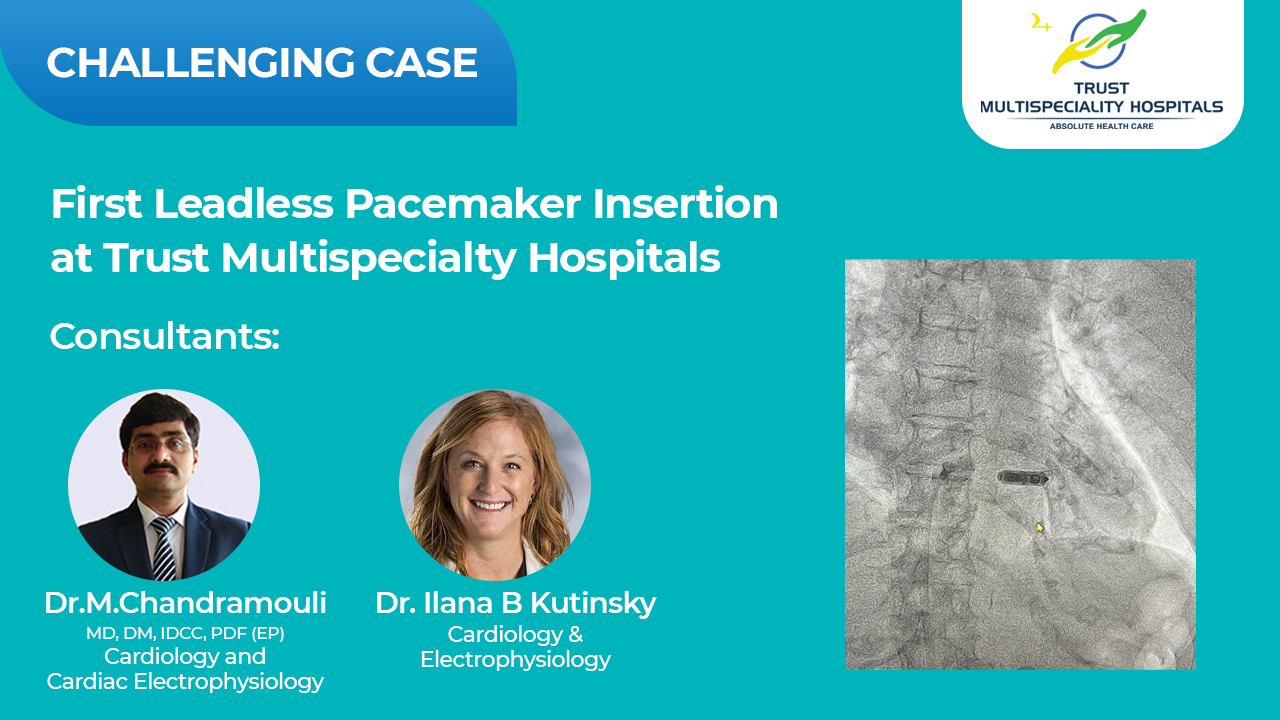
* EP mapping & Ablation
* Pacemaker & ICD implantation
* Structural heart interventions (as per case mix)
⸻
Eligibility
MD / DNB in General Medicine (from MCI/NMC-recognized institution)
Full-time, 3-year residential programme
⸻
For Applications & Enquiries
Apply with CV & contact details
Mention: “DNB Cardiology Application”
+91 98491 35721 (Dr PV Nishanth)
+91 93999 92787 (Dr Pavan Kumar)
Trust Multispeciality Hospitals, Sarpavaram Junction, Kakinada
⸻
Train at a centre where every heartbeat matters
Trust Multispeciality Hospitals — Absolute Cardiac Excellence